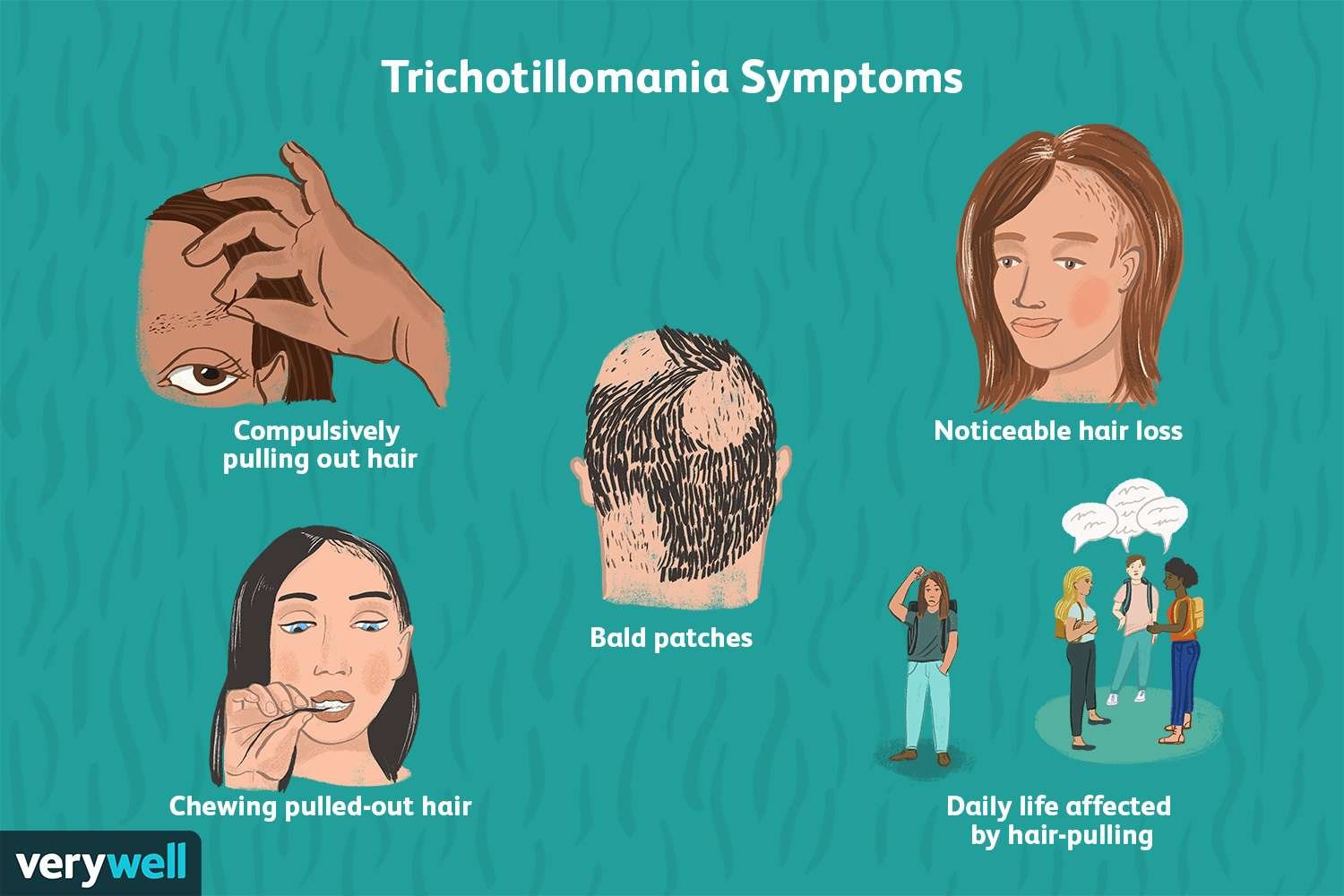
Trichotillomania is a mental health disorder characterized by the uncontrollable urge to pull out one’s own hair. This behavior can cause distress and impact daily life. Effective treatments focus on managing these urges and improving overall well-being.
Habit reversal training is the primary treatment, teaching individuals to recognize triggers and replace hair-pulling with alternative behaviors. Alongside therapy, medications may also be used to help reduce symptoms, especially when comorbid conditions are present.
Early diagnosis and consistent treatment can help control the disorder’s chronic nature. Understanding the options available empowers those affected to take meaningful steps toward managing trichotillomania.
Evidence-Based Treatment Options
Effective treatment for trichotillomania targets both behavioral patterns and underlying triggers. Approaches include structured therapies focusing on habit modification and, in some cases, medications designed to reduce urges or address related psychiatric symptoms.
Cognitive Behavioral Therapy Approaches
Cognitive Behavioral Therapy (CBT) is a first-line treatment for trichotillomania. It works by helping individuals identify and challenge cognitive distortions that contribute to hair-pulling behaviors. CBT also targets the development of alternative coping skills to replace the impulse.
Therapists guide patients through recognizing specific triggers and emotional states that precede hair pulling. Techniques often involve self-monitoring, cognitive restructuring, and stress management. Research consistently shows CBT reduces hair-pulling frequency and improves patients’ control over urges.
Habit Reversal Training Techniques
Habit Reversal Training (HRT) is a structured behavioral intervention grounded in cognitive-behavioral principles. It involves increasing awareness of hair-pulling episodes and teaching competing responses to interrupt these urges.
HRT typically includes several steps: awareness training, development of a competing response (e.g., clenching fists), and building motivation through social support or self-monitoring. Stimulus control methods, such as modifying the environment to reduce triggers, are also incorporated. Studies highlight HRT’s efficacy in reducing hair pulling when practiced consistently.
Medication Interventions
Medication can serve as an adjunct to behavioral therapies but is not universally effective alone. Common pharmacological options include selective serotonin reuptake inhibitors (SSRIs) and N-acetylcysteine, which may reduce symptoms by modulating neurochemical pathways involved in impulse control.
Due to variable response and potential side effects, medication is often reserved for severe cases or those with comorbid conditions like depression or anxiety. Clinicians should weigh benefits against adverse effects and monitor patients closely when prescribing pharmacotherapy. Further research is needed to establish standardized medication protocols.
Supportive Strategies for Managing Trichotillomania
Managing trichotillomania effectively often demands consistent effort and practical strategies. These strategies focus on modifying daily routines, developing coping mechanisms, and leveraging social support to reduce hair-pulling behaviors.
Lifestyle Modifications
Lifestyle changes can help reduce triggers and promote healthier habits. Regular sleep patterns and balanced nutrition have shown benefits for emotional regulation, which may lessen urges to pull hair.
Integrating stress management techniques like mindfulness or exercise can lower anxiety, often a major trigger. Structuring daily activities to keep hands busy with tasks such as knitting or drawing may provide a physical barrier to pulling.
A calm, organized environment with minimal distractions supports focus and reduces impulsivity. Avoiding known triggers, like certain fabrics or stressful situations, also contributes to improved control.
Coping Skills and Self-Help Tools
Effective coping skills help individuals recognize and respond to urges before pulling. Habit reversal training (HRT) is widely recommended; it teaches awareness of pulling behaviors and introduces competing actions.
Other tools include tracking episodes to identify patterns and introducing positive reinforcement for pulling-free periods. Relaxation exercises, such as deep breathing, help manage anxiety and decrease the intensity of urges.
Creating a personalized self-help plan that combines multiple techniques increases success. Mobile apps and guided journals can assist in monitoring progress and strengthening coping responses through daily practice.
Family and Community Support Resources
Support from family and communities plays https://deltanative.com a crucial role in managing trichotillomania. Educating family members about the condition fosters empathy and reduces misunderstandings or judgment.
Peer support groups provide a safe space for sharing experiences, encouraging accountability, and learning new coping strategies. Professional support, including counseling or therapy, reinforces treatment and offers guidance tailored to individual needs.
Families can also help by creating an encouraging environment, helping avoid triggers, and promoting healthy routines. Involvement in support networks encourages consistency and reduces feelings of isolation.